Perhaps everyone has heard about tick-borne encephalitis, however, even today you can hear many myths about this disease. For example, in Siberia, people massively buy insurance against a tick bite, which includes an injection of immunoglobulin; use agents such as iodantipyrine or anaferon; in the end, they decide that it is enough to simply get the tick and cauterize the bite site.
This article is not a guide to the prevention and treatment of tick-borne encephalitis. In the event that you have been bitten by a tick, you must first see a doctor.
Most of the material presented below can be found on the blog of the doctor and popularizer of medicine Alexei Yakovlev (whose work served as the inspiration for writing this article).
Classification
The classification of encephalitis reflects the etiological factors, associated clinical manifestations and features of the course.
The timing of occurrence is distinguished:
- primary encephalitis (viral, microbial and rickettsial)
- secondary (post-exanthemic, post-vaccination, bacterial and parasitic, demyelinating). The second type occurs against the background of various diseases (influenza, toxoplasmosis, measles, osteomyelitis, etc.)
Depending on the presence of inflammation of the meningeal membranes (membranes of the brain), the following forms of encephalitis are distinguished:
- isolated - the clinic has symptoms of only encephalitis;
- meningoencephalitis - in the clinic there are also symptoms of inflammation of the meninges of the brain.
By localization:
- cortical;
- subcortical;
- stem;
- damage to the cerebellum.
By the rate of development and course:
- fast;
- spicy;
- subacute;
- chronic;
- recurrent.
By severity:
- moderate severity;
- heavy;
- extremely difficult.
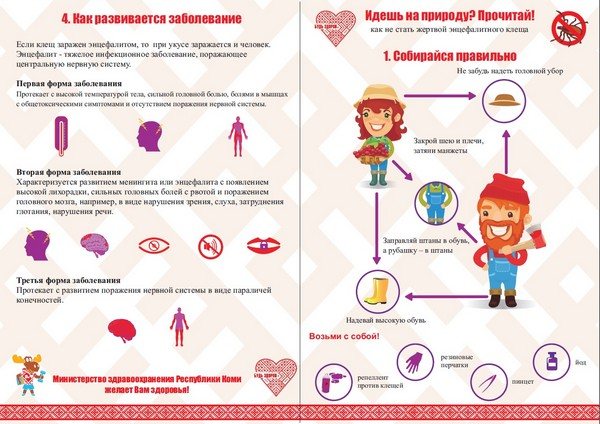
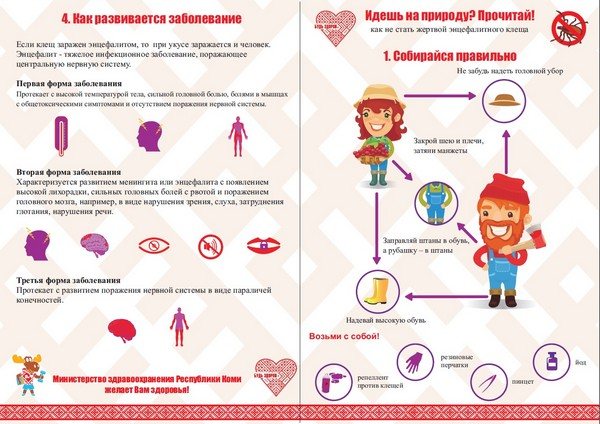
How do symptoms appear when tick-borne encephalitis occurs?
On average, the incubation (latent) period of development of the tick-borne encephalitis virus in the body takes about two weeks. Each form of the disease is characterized by its own symptoms, but the initial signs of infection can be common:
- chills;
- muscle weakness;
- headaches;
- nausea with gusts of vomiting;
- paroxysms;
- increase in overall body temperature;
- redness of the skin on the face and neck, as well as the whites of the eyes.

As tick-borne encephalitis develops, it becomes more characteristic of a particular form of it.
Symptoms of a febrile form
The patient has a feverish state that lasts up to ten days. The characteristic signs of this form of the disease include general weakness, headache and nausea. Neurological signs are poorly expressed. After 10 days, the patient's condition improves, but excessive sweating, an accelerated heart rate and weakness can continue for a month.
Symptoms of the meningeal form
After 3-4 days after the virus enters the body, the patient develops signs of meningitis (damage to the membranes of the brain and spinal cord). In this case, the patient can observe the following clinical symptoms:
- Strong headache;
- vomiting;
- increased sensitivity of the skin;
- muscle tension in the back of the head;
- the inability to unbend the knees on their own.
Signs of meningeal syndrome can last for two weeks, and weakness in muscle tissues after, intolerance to bright light and external stimuli last for two months.
Meningoencephalitic form
In the first two weeks, the patient experiences a two-wave temperature reaction. During the first wave, toxic symptoms occur, and with the onset of the second, meningeal and cerebral symptoms. In the absence of complications, the patient's cure is observed soon, and the course of this form of tick-borne encephalitis is favorable.
Poliomyelitis form
It is diagnosed in 30% of all cases of tick-borne encephalitis. It is characterized by general weakness of the body during the first two days after infection. The polio form of the disease causes the following symptoms:
- weakness in the limbs;
- numbness;
- neck pain;
- inability to keep the head upright;
- limited hand mobility.
Musculoskeletal system pathologies progress within 7-10 days. From the second to the end of the third week of development, muscle tissue gradually atrophies.
Polyradiculoneuritic form
It is rare, no more than 4% of all diagnosed cases of tick-borne encephalitis. In addition to signs of meningitis, during the development of this form of viral lesions, tingling sensations in the extremities and increased sensitivity of the fingers occur. If signs of encephalitis appear after an insect bite, you need to seek medical attention before the nervous system is affected.
Preventive actions
The most effective way to prevent tick bite diseases is vaccination. Especially to people at risk - living in unfavorable areas or near a forest belt.
Six types of vaccines are officially used on the territory of our country, and two of them are intended for children. It is best to vaccinate in late autumn. However, there are also emergency vaccination schedules for emergencies.
In the warm period of the year, vaccinations can also be done, but with such a condition that after vaccination, a person will not visit places where insects live for a month. The effect of vaccination will come only after the specified period. After this time, a re-vaccination is done. Then you can be vaccinated every three years. If, for some reason, the period between vaccinations exceeds 5 years, then the double vaccination will have to be repeated.
Tick-borne encephalitis treatment
Mode. Diet
A strict bed rest is shown, regardless of the general condition and well-being during the entire febrile period and 7 days after the temperature has returned to normal. No special diet required (common table). During the febrile period, a plentiful drink is recommended: fruit drinks, juices, hydrocarbonate mineral waters.
Drug treatment
Etiotropic treatment is prescribed to all patients with tick-borne encephalitis, regardless of previous vaccination or the use of antiencephalitis immunoglobulin for prophylactic purposes.
Depending on the form of the disease, immunoglobulin against tick-borne encephalitis is administered intramuscularly in the following doses.
• Patients with a febrile form: daily in a single dose of 0.1 ml / kg, for 3-5 days until the regression of general infectious symptoms (improvement of the general condition, disappearance of fever). The course dose for adults is at least 21 ml of the drug. • Patients with meningeal form: daily in a single dose of 0.1 ml / kg 2 times a day with an interval of 10-12 hours for at least 5 days until the patient's general condition improves. Heading average dose - 70-130 ml.• Patients with focal forms: daily in a single dose of 0.1 ml / kg 2-3 times a day at intervals of 8-12 hours for at least 5-6 days until the temperature drops and the neurological symptoms stabilize. The course average dose for an adult is at least 80-150 ml of immunoglobulin. • In an extremely severe course of the disease, a single dose of the drug can be increased to 0.15 ml / kg.
The effectiveness of the use of interferon alpha-2 preparations and inducers of endogenous interferon in the acute period has not been sufficiently studied. Ribonuclease is prescribed intramuscularly at 30 mg every 4 hours for 5 days.
Non-specific therapeutic measures are aimed at combating general intoxication, cerebral edema, intracranial hypertension, bulbar disorders. Recommended dehydrating agents (loop diuretics, mannitol), 5% glucose solution, polyionic solutions; for respiratory disorders - mechanical ventilation, oxygen inhalation; to reduce acidosis - 4% sodium bicarbonate solution. With meningoencephalitic, poliomyelitic and polyradiculoneuritic forms of the disease, glucocorticoids are prescribed.
Prednisolone is used in tablets at the rate of 1.5–2 mg / kg per day in equal doses in 4–6 doses for 5–6 days, then the dose is gradually reduced by 5 mg every 3 days (the course of treatment is 10–14 days). For bulbar disorders and disorders of consciousness, prednisolone is administered parenterally. With convulsive syndrome, anticonvulsants are prescribed: phenobarbital, primidone, benzobarbital, valproic acid, diazepam. In severe cases, antibiotic therapy is performed to prevent bacterial complications.
Protease inhibitors are used: aprotinin. The chronic form of tick-borne encephalitis is difficult to treat, the effectiveness of specific drugs is much lower than in the acute period. General strengthening therapy is recommended, glucocorticoids in short courses (up to 2 weeks) at the rate of 1.5 mg / kg of prednisolone. Of the anticonvulsants for Kozhevnikovsky epilepsy, benzobarbital, phenobarbital, primidone are used. It is advisable to prescribe vitamins, especially group B, with peripheral paralysis - anticholinesterase agents (neostigmine methyl sulfate, ambenonium chloride, pyridostigmine bromide).
Complementary treatments
In the acute period, physical activity, balneotherapy, exercise therapy, massive electrical procedures are excluded. Sanatorium treatment is carried out no earlier than 3–6 months after discharge from the hospital in sanatoriums of a climatic and restorative profile.
Tick-borne encephalitis: symptoms and main forms of the disease


Most patients have a febrile form of encephalitis, which is accompanied by the symptoms described above. However, there are other types of encephalitis:
- In the meningeal form, in addition to fever, the patient also develops some of the main symptoms of meningitis. In particular, it is a constant headache, which is accompanied by frequent vomiting. In addition, a stiff neck develops. When performing a lumbar puncture, you may notice that the cerebrospinal fluid flows out under pressure. After therapy, weakness and headaches can bother the patient for another 6-8 weeks.
- In about 10-20% of cases, patients are diagnosed with a meningoencephalic form of the disease, which, as a rule, is difficult. In this case, large foci of inflammation are formed in the brain, which is accompanied by the manifestation of vivid neurological disorders. In particular, the patient may notice some disturbances of consciousness, sometimes even up to stupor. Muscle cramps are possible. Severe weakness of the upper and lower extremities, the inability to move them are also signs of tick-borne encephalitis. In severe cases, the patient falls into a coma. For 20-30% of patients, this form of the disease ends in death.
- The poliomyelitis-like form of the disease is characterized by the development of flaccid paralysis, and the muscles of the neck, shoulders and upper limbs are mainly affected. Tendon reflexes disappear. Approximately 2-4 days, “falling arm” or “hanging head” syndromes appear. Atrophy of muscle tissue gradually develops. In about 50% of cases, this disease leads to the development of disability.
- There is also polyradiculoneuritic tick-borne encephalitis. Symptoms of the disease are paresis and paralysis, which often persist even after full therapy. With this form of the disease, the virus mainly affects the peripheral nerves.
- In modern medicine, the so-called two-wave encephalitis is quite common. What is the peculiarity of his clinical picture? After the latency period has elapsed, the patient experiences the first wave of fever. Quite often it is confused with the common cold, since there are no characteristic symptoms other than high fever and weakness. The fever then disappears, sometimes even for several weeks. This is followed by a second wave, in which the main signs of brain damage appear.
As you can see, the signs of this disease can be completely different. Some forms of encephalitis are difficult to diagnose
That is why it is extremely important to consult a doctor on time, preferably even before the appearance of disorders from the nervous system. The earlier therapy is started, the less likely it is to develop certain complications.
Tick-borne encephalitis virus
The causative agent of this disease is a virus of the genus Flaviviruses. Its size is so small (3-4 times smaller than the measles virus and half the size of the influenza virus) that it easily overcomes all the protective barriers of the immune system.
Tick-borne encephalitis virus has the following features. It is not resistant to ultraviolet radiation as well as disinfectants and high temperatures. When boiled, it dies after two minutes and hot sunny weather for him is also fatal. But low temperatures, on the contrary, support its viability. For example, being in dairy products, flavirus retains its properties for two months.
The tick-borne encephalitis virus lives in the body of the ixodid tick. It can affect both humans and domestic animals, including goats and cows. Infection occurs directly - through a bite or when unsuccessful extraction (if you accidentally crush a tick) or when eating dairy products and milk obtained from infected animals and not heat-treated.
Tick-borne encephalitis can occur in three forms, depending on the symptoms of the disease, which are most pronounced:
- focal (the brain substance is involved in the process and focal neurological symptoms develop), is detected in 20% of victims;
- meningeal (the membrane of the spinal cord and brain is affected), occurs in 30% of patients;
- febrile (fever prevails), occurs in 50% of cases.
Taiga tick
In terms of appearance, this view is practically no different from the previous view. The only difference is the red color of the abdomen when the individual is in a hungry state. Already at the larval stage, it needs nutrition. Most often, rodents become its victims. And since the larva is already attacking the victims, accordingly at this stage it is dangerous.


When an adult is infected, it gives birth to an already infected offspring. Therefore, it is necessary to be afraid not only of adult ticks, but also of individuals at the stage of development of nymphs and larvae.
Classification and stages of development of tick-borne encephalitis
According to the clinical form:
- Acute tick-borne encephalitis:
- Inaparent (latent) form - identification of specific markers of infection in the blood in the absence or minimal severity of clinical manifestations.
- Feverish form - a sudden increase in body temperature to 38-39-С, nausea, sometimes vomiting, increased tone of the occipital muscles without changes in the composition of the cerebrospinal fluid (meningismus), general weakness, sweating lasting about a week. As a rule, it ends favorably, after an average duration of asthenovegetative syndrome is possible.
- Meningeal form (the most common manifest form) - the occurrence of all manifestations of the febrile form with the addition of pathological symptoms of irritation of the meninges, severe toxicosis. Sometimes, with the addition of transient diffuse neurological symptoms, there is a change in tendon reflexes, anisoreflexia (dissimilarity of reflexes), facial asymmetry, and more. Changes in cerebrospinal fluid are characterized by an increase in intracranial pressure up to 300 mm of water. Art., lymphocytic pleocytosis is detected up to 300-900 cells in 1 μl, the protein level rises to 0.6 g / l, the sugar content does not change. In general, the duration of the disease is about 20 days, more often it proceeds favorably, residual effects in the form of intracranial hypertension, headaches, subfebrile condition up to 2-3 months are possible.
- Meningoencephalitic (focal and diffuse) form is a severe, life-threatening form of the disease. With diffuse lesion, toxic and cerebral symptoms, the development of seizures, impaired consciousness of varying severity, sometimes to a coma, come to the fore. With focal lesions against the background of general cerebral and toxic symptoms, motor disorders develop - central paresis (as a rule, completely reversible).
- Polioencephalitic form - disorders of swallowing, drinking, speech, various visual impairments, sometimes twitching of the tongue, when trying to drink water pours out through the nose, paresis of the soft palate is possible. Typical manifestations are respiratory disorders of the central type, vascular collapse and cardiac paralysis, which leads to death. With a favorable course, a long (sometimes more than a year) asthenic syndrome is characteristic.
- The polioencephalomyelic form is an extremely severe course, characterized by damage to the cranial nerves, heart and respiratory paralysis with a mortality rate of up to 30%. In other cases, there is a high probability of paralysis and the transition of the disease to a chronic form.
- Poliomyelitis form - flaccid paralysis of the muscles of the neck, shoulder girdle and upper limbs, periodic disturbances in the sensitivity of these areas, atony. Very indicative of the so-called. drooping head syndrome, when the patient cannot keep his head upright. Sometimes, due to damage to the diaphragm, breathing suffers, which is quite dangerous. The course of this form is long, the restoration of the function of the affected sections does not always take place in full.
- A two-wave course with an indication of the shape of the second wave - the first wave of fever during a week with a complex of cerebral and intoxication disorders, then a period of imaginary well-being lasting 1-2 weeks, and the onset of a second wave of increased body temperature, accompanied by the development of meningeal and focal symptoms, usually without severe consequences.
- Chronic tick-borne encephalitis:
- Hyperkinetic form - Kozhevnikov's epilepsy, myoclonus-epilepsy, hyperkinetic syndrome.
- Amyotrophic form - poliomyelitis and encephalopoliomyelitis syndrome, as well as multiple encephalomyelitis syndrome and amyotrophic lateral sclerosis.
- Rare syndromes.
With the course of the disease is:
- acute - 1-2 months;
- acute lingering (progredient) - up to 6 months;
- chronic - more than 6 months,
Chronic tick-borne encephalitis is caused by the long-term presence of the tick-borne encephalitis virus in the body.More often it develops in childhood and young age. There are four forms:
- initial - continuation of the acute process;
- early - during the first year;
- late - after a year from the acute form;
- spontaneous - without an acute period.
The severity of tick-borne encephalitis:
- easy - with preservation of the ability to work;
- moderate - disability of the III group with partial retention of the ability to work;
- severe - disability of groups I and II, often lack of ability to work.
Possible complications
In a mild form accompanied by fever, complications are usually absent. Also, the meningeal form does not cause dangerous consequences.
With all other forms of virus damage, serious complications may develop:
- speech disorders;
- paresis of the limbs;
- partial paralysis;
- amyotrophy;
- breathing problems.
Severe forms lead to disability in children and adults. Such consequences of an encephalitis tick bite are not cured. In case of insufficient treatment, a lethal outcome is possible. The severity of the consequences depends on the patient's own immune defense.
In case of infection of children, the risks of complications increase manifold due to the weak immunity of the growing organism. About 10% of cases of infection with encephalitis in children are fatal.
What is tick-borne encephalitis TBE
Tick-borne encephalitis is an inflammatory disease of the brain and / or spinal cord of an infectious nature, which develops as a result of being bitten by a virus carrier tick.
Other names for the disease are spring-summer tick-borne meningoencephalitis, tick-borne viral encephalitis, TBE or TVE.
The causative agent of the disease is the arbovirus Tick-borne encephalitis virus, belonging to the genus Flavivirus, which is carried by ixodid ticks of the species Ixodes persulcatus and Ixodes ricinus.
The main signs of the disease are neurological (paresis, convulsions, headache, photophobia, discoordination of movements) and mental disorders, persistent intoxication, fever, and even death.
Diagnosis is based on PCR of blood and cerebrospinal fluid.
Treatment mainly includes administration of immunoglobulin, antiviral drugs, and symptomatic therapy.
The main regions of distribution of encephalitis ticks are Siberia, East Asia and Eastern Europe, where there are forests.
Pathogenesis and periods of tick-borne encephalitis
The incubation period for EC is from 2 to 35 days.
The most vulnerable to tick-borne infection are subcortical nodes and cerebral cortex, cells of the meninges, structures of the bottom of the third ventricle.
Penetrating into the body, the flavivirus infection is adsorbed on the surface of immune cells - macrophages, after which the virus penetrates into them, where the replication of RNA, capsid proteins and the formation of the virion are carried out. Then the viruses leave the cell through the modified membranes and are directed to the perionic lymph nodes, liver cells, spleen, and settle on the inner walls (endothelium) of blood vessels. This is the second period of virus replication.
The next stage of damage to the body by CE is the penetration of the virus into the neurons of the cervical spinal cord, soft tissue cells of the meninges and cerebellum.
Further, the processes of decay of axial cylinders and demyelination, atrophy and destruction of neurons develop. Edema of the brain and spinal cord appears, as well as increased permeability of the walls of blood vessels, which leads to the proliferation of microglia cells and unauthorized hemorrhages.
After that, cerebrospinal fluid (CSF) disorders develop - a condition when the secretion and circulation of cerebrospinal fluid (CSF) is disrupted, as well as its interaction with the circulatory system.In the pathological process, diffuse infiltration of nerve tissues by mononuclear cells, polynuclear cells and plasma cells can be observed, especially in the perivascular space.
Histological studies do not have a clear picture of changes in CE.
Distribution regions and statistics
According to the WHO, about 12,000 cases of TBE are recorded every year. Of these, about 10% falls on the regions of Russia, mainly Siberia, the Urals, Altai, Buryatia, Perm Territory.
The percentage of those bitten by ticks and the detection of EC does not exceed - 0.4-0.7%
Among other regions where the most bites and cases of TBE are recorded are Northern, Central and Eastern Europe, Mongolia, China, and others, where there are large forests.
Next, consider the map of Russia, where the largest number of FEs was revealed:


Prophylaxis
Allocate specific and non-specific prophylaxis of viral tick-borne encephalitis.
Primary non-specific prevention is aimed at eliminating the root cause - a tick bite. To do this, before the start of the warm season (from about mid-spring), the area is treated with special anti-mite preparations, repeating it at regular intervals. Such measures are usually used on the territory of sanatoriums, kindergartens, schools, camps, parks.
Personal non-specific prophylaxis is, first of all, regular self-examination and mutual examination of open parts of the body, scalp and large natural skin folds while being in nature (including in a forest park and a city park). This allows you to detect and remove a tick that has fallen on the skin even before it is sucked.
When going out into nature, closed clothing is preferable, which will make it difficult for the tick to get on the skin. Wide-brimmed hats or hoods are also recommended. And to repel insects, you can use special products that are applied to the skin or clothing.
Specific prevention of tick-borne encephalitis includes:
- Routine immunization of the population using tissue culture vaccine. It is advisable to start it after the end of the warm season - for example, in the middle lane, the first vaccine is usually administered in October-December. After 4, 6 and 12 months, revaccinations are necessary to maintain a sufficient level of the specific immune response.
- Urgent seroprophylaxis, with the introduction of a homologous donor immunoglobulin. The injection is carried out twice - immediately before entering the zone that is epidemically dangerous for encephalitis (the so-called pre-exposure immunoprophylaxis) and within 24 hours after leaving it (post-exposure, that is, after a possible tick bite).
Despite the effective preventive measures developed in the middle of the last century and the achievements of modern pharmacology, viral encephalitis is still considered a formidable infection.
Infection with parasites
Of course, nature has not created them with a dangerous disease, they get an infection through the blood when they attack a sick animal. For this reason, not all individuals are dangerous carriers. Also, as mentioned earlier, the new generation may already have the encephalitis virus, even if they did not feed on blood. This happens when the offspring is laid by an infected female.


Outwardly, it is impossible to determine whether the parasite is a carrier of the virus or not. In order to find out whether a tick that has adhered to the body is dangerous, special studies can be carried out. For this, the sucked parasite must be carefully removed from the body and placed in any airtight container. Then take it to the laboratory for analysis.
What is encephalitis
Encephalitis (Latin encephalitis - brain inflammation) is the name of a whole group of inflammatory processes that affect the human brain, appearing against the background of exposure to infectious pathogens and allergic agents, toxic substances.
Changes in the nervous tissue during encephalitis are rather stereotyped, and only in some cases can we detect signs of a specific disease (rabies, for example). The significance for the body and the consequences of any inflammatory changes in the brain are always serious, so there is no need to remind you of their danger once again.
In the acute stage in the substance of the brain, it causes an inflammatory process, affecting the hypothalamus, basal nuclei, nuclei of the oculomotor nerves. In the chronic stage, a toxic - degenerative process develops, most pronounced in the substantia nigra and pallidum.
In the case of encephalitis of any etiology, complex therapy is required. As a rule, it includes etiotropic treatment (antiviral, antibacterial, antiallergic), dehydration, fluid therapy, anti-inflammatory treatment, vascular and neuroprotective therapy, symptomatic treatment.
Prevention
The most effective prevention against tick-borne encephalitis is considered to be vaccination, which prevents the development of the virus. Vaccination is not an obligatory outpatient procedure. It is assigned to people and pets in such cases:
- The place of residence belongs to an increased risk of infection.
- Frequent trips to the forest.
- The field of activity is related to nature.
- Dogs participate in hunting animals.
- Frequent walks of cats outside the house in the countryside.
Prevention of encephalitis also requires compliance with the rules of stay in the forest. When you are in nature, you should adhere to the following requirements:
- Clothing must completely cover the human body.
- Long sleeves are recommended to be tucked into gloves, and trousers into socks.
- It is imperative to cover your head with a hat.
- Treat the outerwear with anti-mite preparations.
After returning from the forest, it is recommended to undress and carefully examine your clothes and body. If an insect is found, you must immediately call an ambulance.
In addition to encephalitis, the tick is a carrier of various kinds of infectious pathogens, which also pose a threat to human health. To reduce the risk of severe consequences of the disease, a medical institution must undergo a complete diagnosis of the body. In this case, the chance for a complete and quick recovery will also increase.
Summing up
Speaking about the danger from these small blood-sucking animals, it is worth saying that not every individual is infected. But if we consider what serious consequences tick-borne encephalitis brings, then every bite is necessary to beware and afraid.
Do not ignore the attack of the tick and hope that it was not infected, you must take all possible actions to prevent serious consequences. Also, do not forget that the further development of events depends on how well you prepared for a walk in nature.
Diagnostics


Diagnosis of tick-borne encephalitis
When making a diagnosis of tick-borne encephalitis, it is necessary to take into account a combination of three factors: clinical manifestations (symptoms), epidemiological data (time of year, whether the vaccine was given, whether there was a tick bite) and laboratory tests (analysis of the tick itself - optional, blood test, analysis cerebrospinal fluid, etc.).
The first thing to do if a tick attacked is to examine the sore spot. The bite of an infected insect is just a red, inflamed wound, and the encephalitis tick itself looks like an ordinary one. Therefore, in any case, urgent prevention of tick-borne encephalitis is needed - to introduce immunoglobulin against the virus, and then do the analysis. The main diagnostic methods that need to be done after a tick bite are:
- Analysis of patient complaints and medical history;
- General examination (analysis of all symptoms in order to identify typical manifestations of tick-borne encephalitis);
- Virological analysis of blood and cerebrospinal fluid;
- Analysis of arbovirus and determination of its particles in physiological fluids;
- Enzyme immunoassay (level of antibodies in the blood);
- General and biochemical blood tests to determine the severity and characteristics of the central nervous system lesions.
Description of ticks
Many people think that ticks are insect species, but actually ticks are arachnids. As mentioned above, there is no separate species that can infect a person with such a dangerous ailment, therefore there is no image of it either.
The tick is called "encephalitis" because it is potentially dangerous to humans. Based on this fact, other species can be considered dangerous. If the facts suggest otherwise, then the risk of contracting the virus is minimal.
Tick-borne encephalitis epidemiology
Tick-borne encephalitis is a natural focal disease. Strains of the Central European variant are widespread in Europe up to the territory of Siberia. Behind the Ural ridge, the Ural-Siberian and East Siberian genotypes of the virus prevail, in the Far East - the Far Eastern variant. The differences in the clinical picture of tick-borne encephalitis in Europe, Siberia and the Far East are most likely associated with the genetic diversity of the pathogen.
The main reservoir and carrier of the virus in nature is ixodid ticks Ixodes persulcatus, xodes ricinus with transphase (larva – nymph – imago) and transovarial transmission of the pathogen. Additional reservoirs of the virus are rodents (chipmunk, field mouse), hares, hedgehogs, birds (thrush, goldfinch, tap dance, finch), predators (wolf, bear), large wild animals (elk, deer). Some farm animals are also susceptible to tick-borne encephalitis virus, among which goats are the most sensitive. Due to the fact that the range of reservoir hosts is wide enough, there is a continuous circulation of the virus in nature.
The tick becomes infected with the virus when bitten by mammals in the viremic phase.
The main route of human infection is transmissible transmission through tick bites. The risk of infection in humans is closely related to tick activity. The seasonal peak of this activity depends on the climatic characteristics of the geographic regions, but is maximum in spring and summer (from April to August). More often people are sick at the age of 20-60 years. The structure of the sick is currently dominated by urban residents. It is also possible to transmit the virus through the alimentary route (when eating raw milk of goats and cows), as well as as a result of crushing a tick when removing it from the human body and, finally, by aerosol when working conditions in laboratories are violated.
The susceptibility to tick-borne encephalitis is high, regardless of gender and age, especially among those who visit the natural focus for the first time. The indigenous population is dominated by subclinical forms of infection (one clinical case per 60 inapparent).
Immunity after suffering tick-borne encephalitis is stable, lifelong.
Virus-neutralizing antibodies remain in the blood of those who have been ill throughout their lives.
The patient as a source of infection for others is not dangerous.
Life cycle
Tick activity begins with the arrival of heat. As soon as frosts give way to above-zero temperatures, the parasites wake up after a long winter sleep and go in search of food.
Regarding the life cycle of these small blood-sucking animals, much depends on external factors. The maximum period of their life is 4 years. They hibernate in the upper layers of the soil, forest floor and other secluded corners.


When they wake up after a long winter, the main goal is to satisfy hunger and reproduce. The peak of their activity is in May-June, but much depends on the weather, so no one can say the exact time interval when they are most aggressive.
These parasites can go without food for a very long time. With regard to their nutrition, they need it in order to continue the population. The female is unable to lay eggs without being saturated with blood. In addition, she needs much more food than the male.If the male can be on the victim's body for several hours, then the female can suck for several days.
How not to get infected Prevention of tick-borne encephalitis
Prevention of tick-borne encephalitis is divided into general and specific. General prevention is individual protection against ticks. To do this, use special clothing, masks, repellents (tick repellents). It is especially important to examine people after walking in forests, park areas, and to remove the tick from the human body as quickly as possible, since the time of blood suction affects the amount of the pathogen in the blood and the severity of the disease. Also, in endemic regions, unboiled milk should be avoided.


The most effective and reliable method is specific prophylaxis. For this, vaccination is used, which is indicated for tick-borne encephalitis in risk groups.
But according to the recommendations of the World Health Organization (WHO), in areas where the disease is highly endemic (that is, when the average incidence rate from vaccinations given is ± 5 cases per 100,000 people per year), implying that there is a high individual risk of infection, it is necessary to vaccinate for all ages and groups, including children.
In cases where the incidence and prevalence of the disease is moderate to low (i.e. the average annual rate over a five-year period is less than 5 cases per 100,000 population), or limited to specific geographic locations, defined outdoor activities, immunization should be targeted at individuals, in in most cases, to cohorts that are at high risk of infection.
People traveling from non-endemic to endemic areas should also be vaccinated if visits to endemic areas involve extensive outdoor activities.
There are several types of vaccines for specific prophylaxis.
Western European vaccines
In Western Europe, two vaccines are available for both adults and pediatric formulations (Encepur adult, Encepur for children - Germany; FSME-IMMUN INJECT - Austria). Despite the fact that these vaccines are based on the European (Western) subtype of the virus, the immune system produces antibodies against all subtypes of the tick-borne encephalitis virus. These vaccines contain a suspension of purified virus that is inactivated with formaldehyde. All of these vaccines provide safe and reliable protection.
Outside of at-risk countries or areas, tick-borne encephalitis vaccines may not be licensed and must be obtained upon special request, as advised by WHO.
Russian vaccines
Inactivated tick-borne encephalitis vaccines (cultured purified dry horse, "Encevir Neo" for children, "Encevir") produced in the Russian Federation are based on the Far Eastern subtype of the virus and multiplied in the primary cells of the chicken embryo.
The use of vaccines in children under 1 year old is recommended only when there is a high risk of infection with tick-borne encephalitis.
Side effects of vaccines
As for side effects, Western European vaccines are rarely characterized by adverse reactions, sometimes there is short-term redness and pain at the injection site in no more than 45% of cases and fever with a temperature above 38 ° C in less than 5-6%. However, none of these reactions are life threatening or serious.
It is reported that Russian vaccines are moderately reactogenic and do not cause serious adverse reactions. Vaccines, which relatively frequently caused fever and allergic reactions, especially in children, were withdrawn from production.
Antiviral medicines
On the territory of the Russian Federation, the following are more often used:
- For adults and children over the age of 14 - "Yodantipirin".
- For small children (up to 14 years old) - "Anaferon" for children.
Advice! If at the right time these drugs are not at hand, then they can be replaced with Cycloferon, Arbidol or Remantadin.
It is advisable to use the drug "Immunoglobulin" only in the first three days.
Emergency prophylaxis - take a tablet of the drug "Doxycycline", but no later than 72 hours: an adult - 200 mg, a child aged 8 years and older - 4 mg per kilogram of weight. It is not recommended to use the drug for small children and pregnant women.
How to identify pathology
Diagnosis can be made on the basis of a confirmed tick bite. The disease is confirmed using special diagnostic methods:
| Research method | What does it reveal? |
| General blood analysis |
|
| General urine analysis | Moderate proteinuria (appearance of protein in the urine), cylindruria (casts in the urine). |
| Lumbar puncture |
|
| Electroencephalogram | It is prescribed to clarify the depth of the lesion of higher nervous activity, with the development of convulsive syndrome, Kozhevnikovskaya epilepsy. |
| CT or MRI of the brain | These methods are recommended for the development of complications (cerebral edema, cerebral hemorrhage). |
| ECHO-KG | It is prescribed to confirm infectious-toxic myocarditis, cardiac arrhythmias of central origin. |
| Virological method | Based on the isolation of viruses from blood, cerebrospinal fluid. The information content of the study is low, about 40%. |
| Express diagnostics (ELISA, RNGA, RSK, RTGA) | A fairly quick method, it allows you to make a preliminary diagnosis. It is based on the identification of specific antiviral antibodies. |
| PCR | The examination is based on the detection of viral RNA in blood, cerebrospinal fluid, dairy products, ticks themselves, and infected animals. |












