Distinguishing an encephalitis tick from an ordinary one is not so easy, however, solving this problem becomes critical if the bite occurred in an epidemiologically unfavorable region. Indeed, if the parasite is encephalitic, then with some probability it, when bitten, could transmit the pathogen of tick-borne encephalitis to a person and, possibly, at the end of the incubation period, the victim will develop a disease with all its formidable symptoms. Considering the mortal danger of this disease, it becomes necessary to undergo an emergency prophylaxis course as soon as possible. And this is difficult, expensive, long, and taking into account the realities of the work of domestic medical institutions, it is also not very pleasant (hardly anyone likes the queues at polyclinics).
If a person is bitten by an uninfected tick, then no complicated actions are required. It is enough to properly remove it from the skin and disinfect the wound. This is much easier than preventing encephalitis, and certainly safer than treating this disease.
So how to determine whether the tick that was removed from the skin is encephalitis or not? Let's figure it out ...
Is it possible to find out by external signs that the parasite is the carrier of the tick-borne encephalitis virus?
It is simply impossible to distinguish an encephalitis tick from one that is not a carrier of infection by its appearance. The presence of a virus in the body of the parasite does not manifest itself in any way outwardly - neither in the shape of the body, nor in color, nor in behavior. Infected ticks have no clear signs of infection.


On a note
If you put an encephalitis tick and a common tick next to each other, and both of them belong to the same species and be at the same stage of development, then it will not be possible to find any external differences between them. Moreover, even a magnifying glass or a microscope will not help to do this, that is, it will not work to distinguish such individuals at home.
In other words, it is impossible to find out whether a tick is encephalitic just in nature. This cannot be done even by an acarologist who is good at identifying the types of ticks and distinguishing them from each other.
The very concept of "encephalitis tick" indicates precisely the infection of a particular individual with the tick-borne encephalitis virus. Many untrained people mistakenly believe that an encephalitis tick is a certain species, all individuals of which are carriers of infection, in contrast to another, "simple" tick, the bite of which is harmless to humans.
In fact, the established vectors of tick-borne encephalitis are 14 species of ixodid ticks, which are quite similar to each other in appearance, but also have certain features of appearance and color, which make it possible to distinguish them from each other and from other species that do not carry the causative agent of the disease. Of these 14 species, the main vectors of infection that infect humans, in the overwhelming majority of cases, are two:
- Dog tick (aka European forest tick);


- and not much different from it Taiga tick.


The first is responsible for cases of infection with encephalitis in Western Europe, Ukraine, Belarus and western Russia (for example, in the Kaliningrad region), the second - in Siberia and the Far East.
This means that a specific species - an encephalitis tick - does not exist.There are several species, morphologically and ecologically different, that can carry the virus.
On the other hand, even the most vicious carriers of the virus are not all contagious.
According to statistics, only about 6% of those species that carry encephalitis are infected. That is, for 15 specimens of these species, which actually belong to the “encephalitic” cohort, only one specimen will really represent an epidemiological danger.


Moreover, according to the same statistics, after being bitten by infected ticks, without taking appropriate measures, only 2 to 6% of bitten people get sick. Therefore, in those regions where there is a risk of contracting tick-borne encephalitis, out of 10 thousand bites, a maximum of 24 will lead to the development of the disease.
On a note
According to statistics collected from hospitals, the average incidence of tick-borne encephalitis among all people bitten and seeking help is approximately 0.50-0.55% (about 5 people per 1000 bitten). Considering the number of people who do not go to the doctor after a bite, in reality this figure is even lower - about the same 0.2-0.3% (20-30 infected per 10,000 bites). For tick-borne borreliosis, this figure is 1.5 times higher - about 1.3% for people who are officially registered when they go to the hospital.
This, in turn, means that the bite of even a tick that is definitely a carrier of the virus does not necessarily lead to infection.
The main conclusion can be drawn: by external signs, it is never possible to say whether a tick is infectious or not, and even more so, it will not be possible to immediately understand whether the parasite has infected a person when bitten. The same is true for cases when the parasite is removed from a pet - by external signs, it will not work to understand whether an infectious tick has bitten a dog or a cat.
Nevertheless, by the appearance of a bloodsucker, one can determine the likelihood (not a fact, but a chance) that he is encephalitic. For this you need:
- Assess the region where the bite occurred;
- Understand that the parasite belongs to the ixodid tick family;
- If possible, determine whether it belongs to the dyad of the main carriers - it is either a dog or a taiga tick.
The photo below shows a tick as an example, which may well be a carrier of the tick-borne encephalitis virus:


Simply put, if it was possible to determine that in an epidemically dangerous area for tick-borne encephalitis, a person was bitten by an ixodic tick, then the probability of infection is no longer zero. If, when examining the parasite, it turned out to recognize a dog or taiga tick in it, then the likelihood of infection is even higher.
Next, we will consider by what signs it is possible to recognize a possible vector of tick-borne encephalitis ...
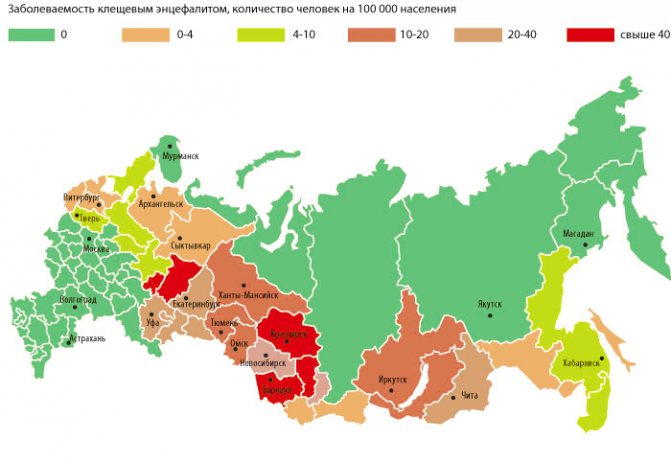
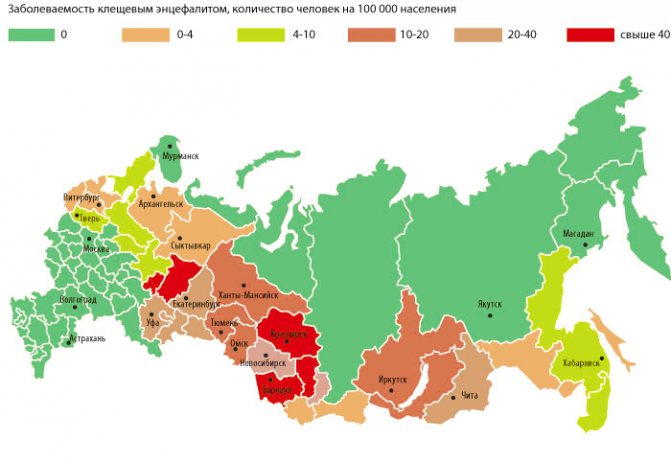
Encephalitis infection statistics in Russia
In 2020, 32 people died from a tick bite followed by infection with encephalitis (according to Rospotrebnadzor). In 2020, 510,000 people received medical assistance who were bitten by ticks. This figure is higher than last year and generally exceeds the average annual values.
Every year from 2010 to 2020, between 29 and 50 deaths from viral tick-borne encephalitis were recorded. For 2020, 29 deaths were recorded, among them there was one child.


The main causes of complications and death from encephalitis are neglect of vaccinations and untimely visits to a doctor. The areas of sanitization are increasing every year, but the number of victims is not decreasing.
44% of those infected with tick-borne encephalitis are people over 50 years old.
In the Moscow region from 2020 to 2020, 41 cases of tick-borne encephalitis were detected, all of them certified by the laboratory. 14 cases were immediately registered when the virus was accidentally brought from other regions of Russia. As statistics show, mostly vacationers catch the infection, leaving to rest in the area in nature.Since 2003, cases of a local nature have also been recorded; for 2015-2017, this figure reached 113 registered cases out of 2873 available. In 2020, the percentage of those infected with encephalitis, namely 62%, fell on the capital of the Russian Federation - Moscow and the region.
According to data for all the past years, a greater number of infected people were noted in the Republic of Tyva. The table shows the statistics with the highest rates.
| Locality of the Russian Federation | % per 100 thousand population |
| Tyva Republic | 23,5 |
| Vologda | 23,04 |
| The Republic of Khakassia | 12,8 |
| Kirov region | 15,07 |
| Sverdlovsk region | 12,2 |
Differences between species of tick-carriers of encephalitis from related species
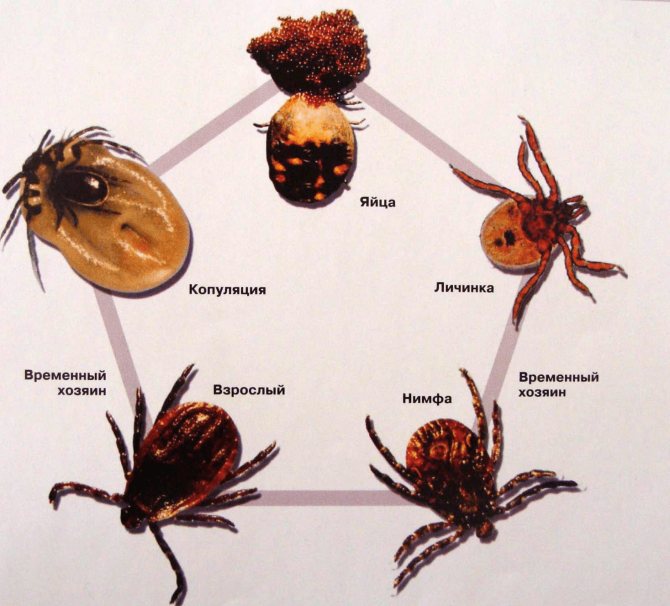
The first task in determining the type of tick in our case is to understand that it belongs precisely to the ixodid tick family. They have a rather characteristic appearance with a body flattened from the back and a very small head. Ticks from other families differ from ixodids in body shape.
For example, the photo shows the Dermacentor silvarum tick, a typical Ixodid that carries encephalitis:


Here is a shell mite from the argas mite family:


And in this photo - Androlaelaps schaeferi gamasid mite:


Only ixodid ticks carry encephalitis. If such a parasite is bitten in a region with a high epidemiological danger, it means that there is a possibility that it could infect a person with a virus.
It is even more likely to become infected by a bite if either a taiga or a dog tick was removed from the body. Outwardly, they are very similar to each other. The photo below shows an adult hungry female taiga tick:
It is also useful to read: When ticks appear and when they disappear


And here is a female dog tick:


It is almost impossible for a non-specialist to distinguish between them, since the reliable differences between them are too insignificant - these are the structural features of the proboscis and the scutellum of the body. But it makes no sense to distinguish between these species: both of them with the same probability can be carriers of infection.
On a note
In the European region, people are attacked mainly by a dog tick, beyond the Urals - by a taiga tick. For this reason, the dog tick is also called the European forest tick, and the taiga tick is called the Siberian tick.
It is possible to distinguish representatives of these two species from relatives by the family of ixodid ticks by their color: taiga and dog ticks in adulthood have a well-visible black or dark green scutellum and a brown body. When saturated, their body increases in size several times and becomes light gray.
You also need to be able to distinguish ticks from some blood-sucking insects. In particular, in the forest and taiga zones, bloodsucking flies can be easily confused with ixodids, the most common and famous of which are the deer bloodsucker (it is also called the elk tick). These flies attack various large animals and humans, and they tend to climb into the hair and move between them. Bloodsuckers pursue their prey in flight, but clinging to wool or skin, they shed their wings and begin to suck blood - such a wingless individual can be easily confused with a tick.
The photo below shows a deer bloodsucker:


And here - the usual forest tick, which has not yet been fed:


The photograph shows the main difference between these arthropods: the bloodsucker has six legs, and the tick has eight.
The main thing: bloodsuckers do not tolerate encephalitis and do not infect a person with any infections at all.
In view of the above, in the case of a tick bite, it can only be assumed with a certain probability whether it can be infected with a virus or not. But in order to find out for sure, completely different research methods will be required ...
The only way to know if an encephalitis tick is or not
Surely it is possible to find out that a tick that has bitten a person is infected with the tick-borne encephalitis virus only by the results of a special laboratory study. The essence of such a study is simple:
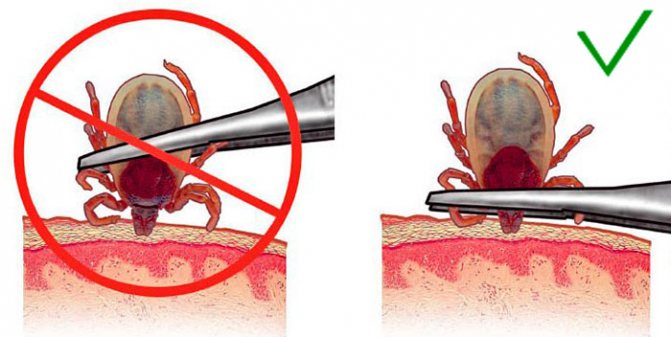
- A bitten person keeps the parasite in any way (preferably alive - this way the analysis can be carried out within a few days after the bite), puts it in an empty bottle, matchbox or even in a plastic bag, and takes it to the laboratory;
- In the laboratory, using special microbiological methods (mainly ELISA test, less often PCR analysis), certain tissues of the parasite are examined and the presence of the pathogen of tick-borne encephalitis in them is revealed;
- If the pathogen is found, it is concluded that the tick is infectious. If the pathogen is not detected, accordingly, the parasite is considered uninfected.


Such research is very effective. It is very easy to detect viral RNA in tick tissues using available and inexpensive methods; such analyzes are carried out in a few hours and give a result with a high degree of accuracy. They also make it possible to determine with a high probability whether a person needs emergency prevention of the disease.
On a note
According to a study carried out in clinics in Irkutsk, prevention of tick-borne encephalitis is actually required only for 12% of people affected by bites, regardless of how many parasites have bitten a particular person. It is clear that the risk of infection will be higher in a hunter or a tourist, from whom several dozen fed ticks were removed, than in a person who was resting in the park and removed from himself one parasite that had just sucked. These figures show that not every bitten person needs urgent measures.
It should be remembered here that even if the bloodsucker is contagious, the likelihood of developing the disease in a person bitten by him without taking any measures is about 2-6%. That is, even after a positive test result for a tick in the laboratory, it is not at all necessary that the disease will develop. Nevertheless, the risk of its development is a sufficient reason for taking emergency measures.
Incubation period
Every year, the number of encephalitis ticks detected by a bite is greater than that of people who contract encephalitis. How to distinguish an encephalitis tick? In the laboratory, or for the consequences of a bite.
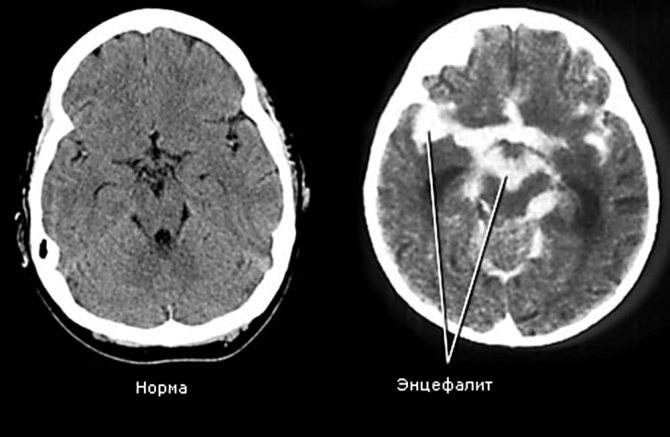
If, nevertheless, an encephalitis tick has bitten, you should pay attention to the incubation period, which lasts up to 2 weeks. In the presence of tick-borne encephalitis, a person develops a fever. The viremic phase lasts 3 days and causes loss of appetite, dyspeptic disorders, migraines, weakness and muscle aches. After that, within 1 week, the stage of remission passes, after which, in 30% of cases, the next phase begins, characterized by disorders in the central nervous system. It can be encephalitis and meningitis.


With meningitis, the patient feels a severe headache, febrile symptoms reach a critical level, and there is a stiff neck muscle. With encephalitis, the patient experiences impaired consciousness, loss of some motor functions, impaired mobility and disorders of the nervous system. First, a temperature of 37 ° C appears, then it rises sharply to 39.
Ticks are most dangerous in the Far East.
The nature of the course of symptoms after an encephalitis tick bite is more dangerous and the disease is expressed by strong symptoms.
In the first hours after a bite, a person's temperature rises to a critical one, headaches and vomiting, insomnia are tormented. After 4-5 days, symptoms of central nervous system damage occur.
In addition to encephalitis and meningitis, a number of diseases can be obtained after being bitten by an infected tick.
How and where to take a tick for analysis
In regions with a high epidemiological danger of tick-borne encephalitis, the analysis of removed ticks for infection is carried out in most laboratories at clinics and hospitals. The method of emergency research of ticks was initially tested in Krasnoyarsk, Irkutsk, Tomsk, Novosibirsk, Omsk and Yaroslavl, and when it showed good results, it was introduced into regular practice in most cities of Russia, Belarus and Ukraine.


You can conduct the analysis itself or find out where you can carry the tick for research in the following institutions (you can call):
- In any polyclinic or hospital (and in rural areas - in a first-aid post or at a local therapist);
- In any emergency room;
- In the nearest department of the Sanitary and Epidemiological Station;
- In private laboratories and diagnostic rooms;
- In the centers of Rospotrebnadzor.
In the event of a bite, it is enough to call any of these institutions and find out where to go. On the phone they will say either the address of the laboratory or its phone number.
On a note
If the victim cannot remove the tick on his own or is afraid to do it, then the doctor in the clinic will be able to carry out all the necessary manipulations and he will hand over the parasite for analysis.
The cost of analyzing a tick for encephalitis ranges from 300 to 700 rubles, depending on the region and the prestige of the clinic (laboratory). A separate analysis of the parasite for the causative agent of Lyme disease will cost about the same, and a comprehensive study on both pathogens costs less than two separate analyzes.
The quality and accuracy of analyzes in both public and private laboratories are the same. The advantage of state institutions is the lower cost of analysis, but in private clinics there are fewer queues, and the whole procedure is more comfortable and faster.
It is also useful to read: Memo for parents on the topic "Caution, ticks!"


The tick must be brought in for analysis as soon as possible. If he is alive, he can be injured when removed from the skin, which will lead to his early death. A dead parasite can be examined for no more than 3 days after death, so if it was killed during removal, it must be taken to the laboratory immediately. If the tick is alive, it must be placed in an airtight container and transported in it for analysis.
The urgency in this case is due to the fact that with confirmed tick infestation, emergency prophylaxis should be started in the first 2-3 days after the bite. Only if it is carried out within these terms, it will provide the desired result and with a high probability will prevent the development of infection. If during this time it was not possible to deliver the parasite for verification, then you can no longer fuss: it does not matter whether it is infected or not, the deadlines have already been missed (however, you still need to try to carry out the research).
The debatable question is whether it is worth carrying out a comprehensive analysis of the parasite for tick-borne encephalitis and borreliosis. The main danger of tick-borne encephalitis is the complexity of its treatment and the absence of highly effective antiviral agents. This is the reason for the high incidence of disability and death in case of illness.
Lyme borreliosis is easier and more successful to treat due to the fact that its pathogen is sensitive to antibiotics.


Therefore, if tick-borne encephalitis is easier and safer to prevent before the development of the disease, and for this it is worthwhile to analyze the tick and emergency prevention, then borreliosis with timely diagnosis is easier to cure. Moreover, the likelihood of infection with a bite is also low. In general, in this matter, it is better to follow the instructions of a specialist who knows the epidemiological situation in the area. If he thinks that the likelihood of contracting Lyme disease is high, then he will advise you to pass a comprehensive analysis. If such an analysis, in his opinion, will not be appropriate, then he will not recommend it.
If the removed tick turned out to be infected with the tick-borne encephalitis virus, then the victim needs the introduction of immunoglobulin as a measure of emergency prevention of the development of the disease. Consultation on further actions will be given by a doctor at the institution in which the study was conducted.
Signs of borreliosis
Along with tick-borne encephalitis, a person can get Lyme disease, or borreliosis. The symptoms of tick-borne encephalitis and borreliosis are similar, and it all starts with a tick bite.After contact with an insect, a person's temperature rises, weakness, myalgia, migraine, and a violation of the central nervous system appear. If, with encephalitis, symptoms appear already in the first day, then borreliosis can give the first symptoms after a few weeks and even after 1 month.
You can tell Lyme disease from encephalitis by looking at the bite site. With borreliosis, at the site of contact of the skin with a tick, erythema occurs, local or multiple, recurrent and migratory. It looks like a pink bright ring with a light area inside. After a tick bite, a person or dog immediately leaves a bright spot.


Signs of CNS damage in tick-borne encephalitis and borreliosis:
- 1 Painful sensations in the neck, shoulders, lower back associated with a violation of the radicular nerves.
- 2 Neuralgia at the site of erythema formation.
- 3 Paresis of the facial nerves on one or both sides of the face.
- 4 Serous meningitis syndrome.
The manifestations of tick-borne encephalitis are similar at first to the symptoms of influenza. In both types of the disease, patients experience lethargy, fever, fever, chills, muscle aches, sometimes vomiting and reaction to light. The manifestations of influenza are distinguished by the presence of a headache in the forehead and temples, the patient experiences pain when blinking and looking around, a sore throat and a cough appears, the nose is stuffy.
What to do if it was not possible to analyze the infection of the parasite?
A situation is possible when it was not possible to deliver the tick for analysis to the laboratory. Therefore, it is impossible to understand whether it is contagious or common. This can happen on a camping trip (it is unlikely that anyone would think of removing a group from the route in Altai if one of the participants was bitten by a tick), on a long hunting trip, on an expedition. Finally, the bitten person can live in a very remote settlement, from where it is extremely difficult to quickly deliver the parasite for analysis.


This also includes the situation when the tick simply did not have time to be delivered for research within 2-3 days after the bite.
What to do in such cases?
Firstly, you no longer need to take a tick for analysis. Even the understanding that he was infected with the tick-borne encephalitis virus or borrelia will not be a reason for urgent measures: the terms of emergency prevention have already been missed, and it is inappropriate to start treatment without symptoms of the disease.
Secondly, there is no need at all costs to carry out emergency prevention of tick-borne encephalitis. If it was not possible to bring the parasite to the hospital in 2-3 days, then most likely it was not possible to inject immunoglobulin within the same time frame. There is no point in introducing it later, since it will not have a pronounced effect.
Thirdly, you need to carefully monitor the condition of the victim. If there are obvious symptoms of either encephalitis or borreliosis, then you need to see a doctor as soon as possible.
Signs of tick-borne encephalitis after a bite develop at different times - depending on the subtype of the virus, usually from 3 to 14 days. The first symptoms of the disease are fever, pain in the head and muscles, chills, and nausea. If they appear, you need to immediately take the victim to the hospital.
It's important to know
For the European subtype of the virus, a special pause is characteristic, when, after 2-3 days of fever, the patient's condition returns to normal, and then brain damage begins with impaired consciousness and even paralysis. If remission is taken for the end of the disease and nothing is done, then you can miss the moment when you can still do without the severe consequences of the disease.
When infected with the Far Eastern subtype of the virus, both phases merge, the general symptoms are more pronounced, the disease progresses very rapidly.
When infected with borreliosis in the acute phase of the disease, fever develops, and erythema migrans - ring-shaped redness around the bite site may also appear.Likewise, if you experience these symptoms, you should see your doctor as soon as possible. If antibiotics are started on time, the disease will most likely be safely cured.


You can also donate a blood test for antibodies to tick-borne encephalitis virus or lime borreliosis. The analysis for immunoglobulins for the TBE virus is given in 2-3 weeks after the bite, and for borreliosis - after 3-4 weeks. It is pointless to take them earlier, because even with infection, the antibody titer will not have time to increase to those values that would be a sign of infection.
Even if the first test for antibodies did not give results, it is useful to repeat it after a month. The dynamics of changes in the titer of antibodies and their composition will be an important sign of infection. If both tests for each infection are negative, then you can calmly take a breath: the infection has not occurred.
When you don't have to worry about tick infestation
Finally, there are situations in which you do not have to worry about tick infestation at all.
For example, it makes no sense to bother to determine the infectiousness of a parasite if it has bitten in a region where encephalitis was either not registered, or only isolated cases of the disease were known.
So, in most of the territory of Ukraine and in the southern regions of the Russian Federation, many mothers go crazy with fear when they find a tick on a child, although in fact the likelihood of infection with TBE is not excluded here, but it is so small that no special measures are required. Almost certainly, the tick here will not be encephalitic and will not infect the victim with a virus.
Further, when traveling to a region with an increased risk of contracting tick-borne encephalitis, an anti-encephalitis vaccine is an elementary safety measure. It ensures that after being bitten, even by an infected parasite, a person does not get sick. If the vaccination is done, then it is not necessary to find out whether the tick is infectious or not. And it is unreasonable to go to such a region without vaccination and then walk through the forest.
If the tick has not yet bitten, but is simply found on the body or on clothes, it is enough to simply brush it off. Without a bite, the virus is not transmitted through the skin, and it is impossible to get infected simply from a parasite crawling on the skin.


Finally, there is no need to worry if, after a walk in nature, a bite is found on the body, but it is not clear who left it. Most likely, this is not a tick, since it sucks blood for a long time - from several hours to several days, and if a bite is found, it is with a sucked parasite.
Be that as it may, in each specific case, after a tick bite, it is most correct to find an opportunity to contact a doctor (preferably an infectious disease specialist) and consult him. He will be able to tell exactly how to be in a specific situation, where and when to seek help. It is much wiser and safer to follow his recommendations than to independently determine the infestation of the tick and draw some conclusions.
Interesting video: how to reliably protect yourself from tick-borne encephalitis
Precautions
- To avoid getting a tick, it is important to protect yourself in advance. Avoid untreated areas of forests and parks, it is advisable not to visit places with high vegetation during periods of activity.
- If you happen to get into such a place, you need to cover all open areas of the body with clothes to the maximum, be sure to wear a hat.


The figure shows the most favorite places where ticks bite.
- You can also use protection, such as repellents, which are sold in any supermarket.
- When you arrive home, be sure to check yourself and your loved ones for ticks. Clothes should be washed in hot water, because the larval forms are invisible to the eye and can reach you already at home.
- If a tick has bitten, take the steps outlined in the previous subheading as soon as possible. In no case should you ignore the symptoms and blame everything on the walking flu, because the first signs of encephalitis at the initial stage are not much different from it, but the consequences are many times worse!
Many ticks are carriers of dangerous diseases. Therefore, it is important to know who bit you and what to do next. In today's article, an encephalitis tick, a photo and its description will be considered.
There will be a lot of photos to have a complete picture of the activity of the bloodsucker in nature, on the human body, its larval stage and bite marks.